National Collaborating Centre for Mental Health
We are delighted to introduce the work of the National Collaborating Centre for Mental Health (NCCMH).
National Collaborating Centre for Mental Health

Foreword
Dr Lade Smith CBE,
Current President of the RCPsych,
Former Clinical and Strategic
Director of the NCCMH
Over more than 20 years the NCCMH has forged an excellent reputation for developing evidence-based guidance, pathways, competence frameworks and quality improvement (QI) collaboratives.
They are led by internationally renowned clinical leaders, and has well-established links and relationships with NHS England and Improvement, the National Institute for Health and Care Effectiveness (NICE), the Care Quality Commission (CQC), and mental health providers and service users across the UK.
At the heart of all the NCCMH's work is a desire to improve mental health services for people and to ensure equitable access. Therefore people with lived experience of mental health problems are a central part of every stage of their processes, as are clinical leaders and front line staff. This means that the work is grounded in the reality of the people who use and provide mental health services and is underpinned by a drive to address health inequality.
The NCCMH works from the evidence base up. They developed NICE guidelines for 15 years and now are involved in the implementation of high-quality evidence.

They work at the service-level to reconceptualise what mental health services look like, by designing pathways and developing guidance
They ensure that the workforce is skilled by developing competence frameworks and curricula
They evaluate new services, training packages and interventions
They support professionals to improve mental health service delivery using a QI approach to ensure sustainable change
They help other countries to adapt or develop evidence-based guidance (including, most recently, Ukraine).
In March 2022 the Public Mental Health Implementation Centre, which is hosted by the NCCMH, was launched in the Houses of Parliament in Westminster. This marks an exciting new chapter for the NCCMH and the College.
The NCCMH are proud to work with a wide range of partners to improve mental health care nationally and internationally and look forward to working with you.



How we work
Co-production and equality
In the NCCMH, all our work is underpinned by our commitment to co-production (working collaboratively with people, without hierarchy) and reducing inequalities in mental health care.
We work with people with lived experience as equal partners when designing and delivering our work, often as early as the bidding process for commissioned work, to ensure the work we propose is co-produced and advances mental health equality. In addition to our own work being co-produced and ensuring there is a focus on equality, we support others to involve people with lived experience and identify disparities around equality in their own work and how to address this, whether that’s in a resource, standards, or through quality improvement support.
To ensure we have a wide range of experiences and views, we have an NCCMH Equality Advisory Group (EAG), a standing committee of people from a diverse range of backgrounds with lived and learned experiences of mental health services in the UK. The EAG supports the NCCMH to adhere to its commitment to actively advance co-production and equality. The group meets regularly to discuss NCCMH projects from a co-production and equalities perspective, often as a critical friend, to advance our work and ensure it results in improvement for as many people as possible in accessing mental healthcare, their experience of the support they receive and their outcomes.


Service design and development
Guidance and care pathways
At the NCCMH, we are committed to encouraging positive changes to mental health service design. We have a tried and tested approach to new service design and development to support health care leaders in service development.
Our freely-available resources include a service design report for young adults services, commissioning guidance for equality in mental health care services and commissioning guidance for co-production.
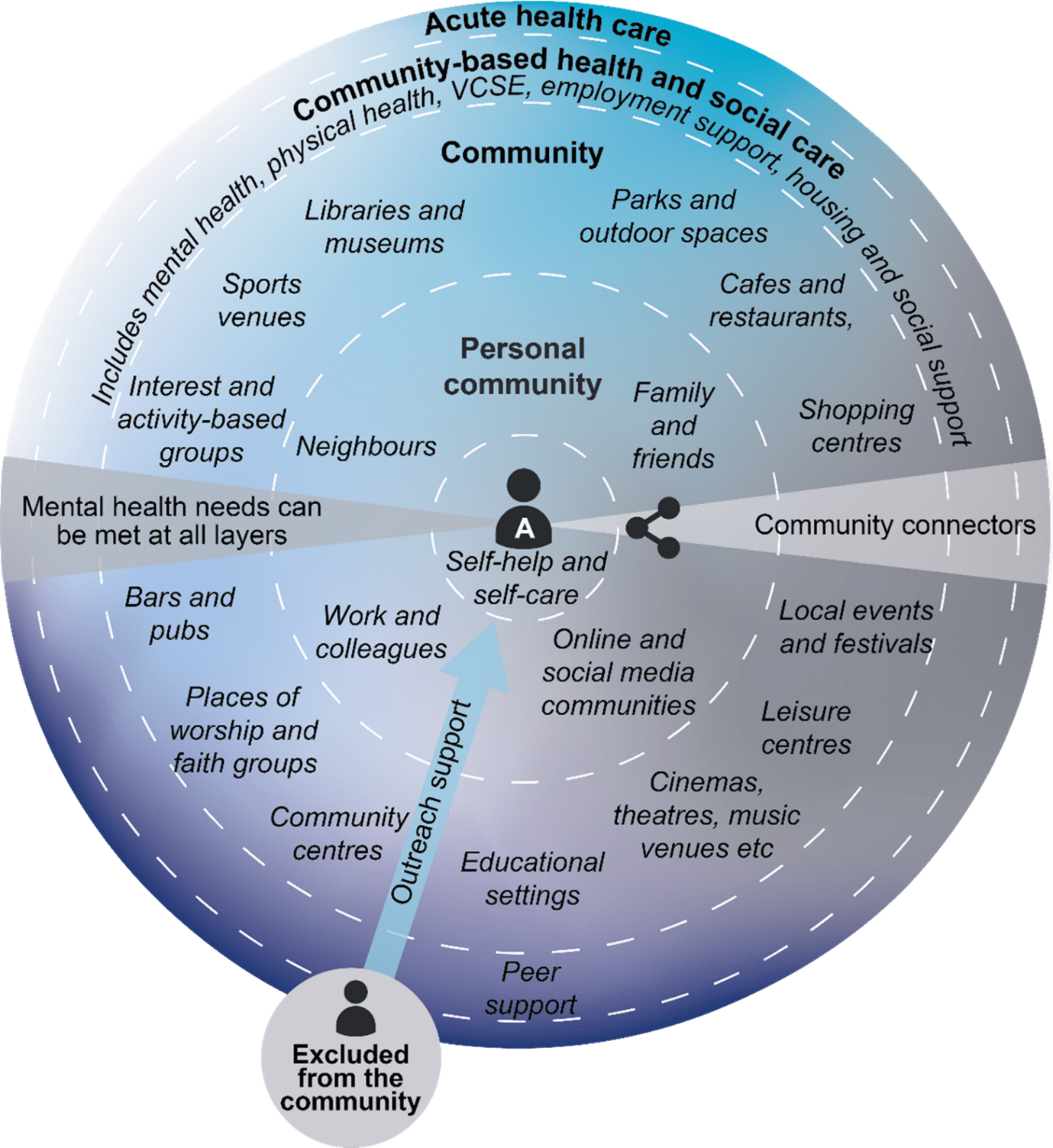
The NCCMH developed the Community Mental Health Framework for NHS England in 2019. It aims to enable the Long Term Plan’s ambition for new and integrated models of primary and community mental health care, which will support adults and older adults with mental health problems, to be achieved.
Since then, the Framework has been implemented across the country, driving the largest national change to community mental health provision in 30 years.
The Framework set out a new structure for place-based community mental health care, which can provide whole-person and whole-population health approaches. At the heart of the Framework is a ‘core’ community mental health service, combining primary care provision with secondary care community mental health teams and residential care. That core is built around existing GP practices, neighbourhoods and community hubs. Implementation of the Framework means that people with mental health problems would be able to:
Access mental health care where and when they need it, and be able to move through the system seamlessly
Have a good quality assessment at whatever point they present, and access evidence-based interventions at the location most suitable to their needs
Step up to more specialist care when needed, including crisis and inpatient care, as well as specialist residential care or dedicated eating disorder services
Access physical health care, advocacy services, community assets (such as libraries, leisure and social activities and faith groups), support groups, employment, education, volunteering and training services, housing and social care services, and help and advice on finances and benefits, when they need them
Manage their condition or move towards individualised recovery on their own terms, surrounded by their families, carers and social networks, and supported in their local community (as pictured in the graphic)
Contribute to and be participants in the communities that sustain them, to whatever extent is comfortable for them
The Framework laid the foundation for NHS England’s Community Mental Health Transformation, which is now fully underway, with the aim of enabling at least 370,000 adults and older adults per year nationally to have greater choice and control over their care, and to live well in their communities.

Quality improvement (QI) programmes
We are proud to showcase an extensive portfolio of high-impact programmes we have delivered across a broad range of mental health services. Areas of focus include staff wellbeing, suicide prevention and reducing restrictive practice. Please see some examples on the right.

Throughout 2021/22 we worked with 38 teams in England and Wales to understand and improve the experience, wellbeing and joy of staff in the Enjoying Work Collaborative. Each week, the teams completed a survey that asked their members three questions based on their experience of work in the past week. The results showed an improvement across the three outcome measures.
Our latest QI collaborative is focused on demand, capacity and flow within inpatient mental health settings and was launched in January 2023. This 18-month project aims to:
support community and inpatient teams within mental health services to understand demand, develop and test change ideas to improve flow, reduce waiting lists and manage demand in creative ways
provide opportunities for peer-to-peer sharing and learning through regular in-person events

In 2018, the NCCMH supported 38 inpatient mental health wards across England to reduce their use of restrictive practice using a QI approach.
In 2021, NHS England commissioned the scale up and spread of the reducing restrictive practice (RRP) pilot as part of the Mental Health Safety Improvement Programme (MH-SIP).
The scale-up aims to take the learning from the pilot, including the main areas pilot teams focused on to reduce restrictive practices and ideas tested, to assist teams as they start working on their own projects.
RRP: Our impact
Since its inception in 2018, participating wards have had numerous success stories.
Wards have been testing over 350 change ideas since the Reducing Restrictive Practice Collaborative started and by February 2020 those ideas resulted in 24 out of 38 wards seeing reductions ranging from 25% to 100% in one or more measure of restrictive practice (number of physical restraints, seclusions and rapid tranquillisation episodes).


Public Mental Health Implementation Centre
Mental disorder accounts for at least a fifth of UK disease burden due to a combination of high prevalence, early onset, and a broad range of associated impacts and inequalities.
Effective interventions exist to treat mental disorders, mitigate associated impacts, prevent mental disorders from arising, and promote wellbeing and resilience.
However, in the UK, only a minority of those with a mental disorder except psychosis receive treatment and far fewer receive interventions to prevent associated impacts.
Furthermore, there is negligible provision of interventions to prevent mental disorder or promote mental wellbeing and resilience.
The public mental health implementation gap results in population-scale preventable suffering, broad impacts and associated economic costs. The gap also breaches the right to health, reflects lack of parity and has further widened with the COVID-19 pandemic.
The Public Mental Health Implementation Centre (PMHIC) aims to support improved implementation of evidence-based interventions to treat mental disorder, prevent mental disorders and associated impacts, and promote mental wellbeing and resilience. This will result in the sustainable and equitable reduction of the impacts of mental disorder and promotion of population mental wellbeing locally, nationally and internationally.
Collaboration and leadership: Support collaboration and leadership on public mental health with many stakeholders.
Public mental health in psychiatry: Promote public mental health as an intrinsic part of psychiatry, and support College members to develop their knowledge and understanding of public mental health.
Education: Work with other professional groups to integrate public mental health training into their teaching programmes.
Evidence: Provide high-quality evidence, advice and recommendations on public mental health to government and other policy-making bodies at local and national levels.
Needs assessment: Support mental health needs assessment at national level to estimate size, impact and cost of implementation gap of effective public mental health interventions taking account of issues such as COVID-19. It will also support translation of needs assessments into improved implementation across populations.
Research: Support identification of public mental health research priorities, including implementation research, given the national and international implementation gap.
Reports and Publications
Since the centre was launched in 2022 we have published a set of publications focused on public mental health. Find out more below:


Clinical guideline development
Since the NCCMH was established in 2001, we have been at the forefront of reviewing evidence and developing gold standard guidelines for mental health.
The NCCMH developed 36 mental health guidelines for NICE that have been translated and adopted/adapted by other public healthcare systems, including in Italy, Australia and Slovenia.
The mental health guidelines were developed from the best research evidence, using predetermined and systematic methods to identify and evaluate the evidence. If there wasn’t enough evidence, consensus statements from the guideline committee were used to form statements and recommendations. These guidelines continue to be referred to by professionals and people using services around the world. Notable guidelines are:
The first-ever NICE guideline (on schizophrenia)
The first guideline on service user experience
The first collaborative guideline with the Social Care Institute for Excellence on dementia.
Our guidelines have led to some important developments in the field of mental health. They have provided the evidence base that has supported:
The National Service Framework
The Improving Access to Psychological Therapies (IAPT) programme for depression and anxiety disorders.


In the past, the NCCMH has provided consultancy to Turkey, Georgia, South Korea and the Netherlands to develop their own clinical guideline programmes, based on the NICE mental health guidelines we developed.
Our approach is to utilise the latest evidence base and learning from the UK, and then work with local experts to tailor the guidance to the specific cultural and economic context our partners and clients are working in.
More recently, we contributed to a project in Lviv in Ukraine to develop a compendium of recommendations on common mental health problems (depression and anxiety disorders) and on severe mental disorders (psychosis, schizophrenia and bipolar disorder). These synopses of NICE recommendations were specifically adapted for the Ukrainian context.

Research
We are regularly commissioned to carry out and publish research into mental health programmes leading to improvement in culture, service configurations and patient care.
Our reports contain recommendations and practical help for mental health services by describing the culture and initiatives of services that lead by example in how they work and what they do.
Systematic reviews
We have published a range of rapid systematic reviews encapsulating all available evidence on a particular topic.
E-therapies for children and young people
Evidence Review – Surge Planning for Mental Health
Severe mental illness and substance misuse
Social class and treatment for mental health problems
Tourette syndrome - treatment for tics in children and adolescents
Evaluations
We carry out evaluations of mental health services and interventions:
Reports
We write reports on specific areas of mental health care, commissioned by other organisations.


Competence frameworks
The NCCMH has collaborated with experts in their fields to develop competence frameworks for staff working in mental health care.
The competence frameworks identify the skills, attitudes, values and knowledge needed by professionals in particular roles. They have been developed in collaboration with a broad range of stakeholders including clinicians, academics, commissioners, service users, families and carers. They are often accompanied by a supporting document (containing background, discussion and evidence) and a training curriculum.
Find out more about each competence framework and download the documents from the links below:
Individual Placement and Support
Inpatient Children and Young People’s Mental Health Care
Mental Health Peer Support Workers
Physician Associates in Mental Health
Find out how to commission us here
Thank you for reading.
National Collaborating Centre For Mental Health
Our team would love to speak to you about what we do.